Aim
The aim of treatment is to remove abnormal cells, allowing the
lining of the oesophagus to grow back with normal cells. The
process of removing dysplastic Barrett's should be considered a
treatment journey, with several individual treatments and
assessments being used together to do our best to get rid of the
Barrett's and prevent cancer, or detect and treat cancer at a very
early stage. This usually involves a number of upper GI endoscopic
treatments which are summarised here and are explained in more
detail below.
- Any nodules or lumpy areas are removed in 'chunks'. This is
called an Endoscopic Mucosal Resection (EMR).
- Other large areas of dysplasia are destroyed using a special
energy device called Radio Frequency Ablation (RFA). This allows
long areas of dysplastic Barrett's oesophagus to be treated.
- Small residual areas of dysplasia or Barrett's oesophagus are
destroyed with a smaller device. This is called Argon Plasma
Coagulation (APC).
After getting rid of the dysplastic Barrett's, further
endoscopies are performed at regular intervals to check for any
re-growth of abnormal cells.
Treatment plan
The overall treatment plan can be broken down into different
phases, called the treatment cycle, the follow-up cycle, and
surveillance. These are shown, along with the associated
procedures, in figure 1.

Figure 1. Dysplastic Barrett's treatment, follow-up and
surveillance. OGD - upper GI endoscopy.
Endoscopic Mucosal Resection (EMR)
The wall of the oesophagus has several layers, as shown in
Figure 2.

Figure 2. Layers of the wall of the oesophagus.
Dysplasia and early cancers are found and limited to the
innermost layer, which is called the mucosa. The mucosa rests on a
layer of connective tissue that carries blood vessels and nerves,
which separates it from the muscle layers of the oesophagus.
Endoscopic mucosal resection (see figures 3-5) involves the removal
of 1-2cm discs of mucosa using an endoscope. Because the endoscope
is inserted and removed several times during the procedure and it
takes longer than a regular endoscopy, we currently perform this
procedure under general anaesthetic in an operating theatre.

Figure 3. Endoscopic mucosal resection procedure.
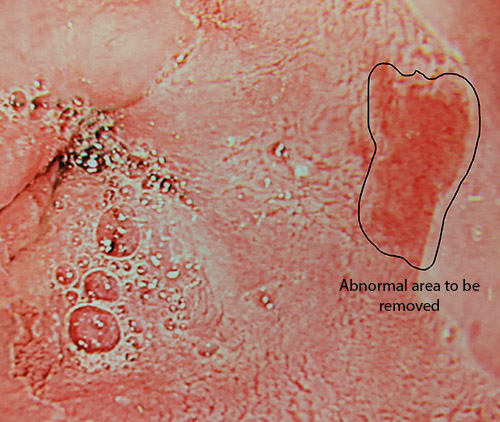
Figure 4. Abnormal area of Barrett's to be removed with EMR
(seen using acetic acid chromoendoscopy). Source: UHBW NHS
Foundation Trust.
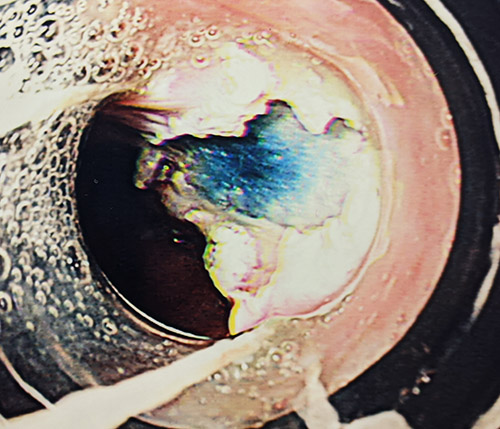
Figure 5. Area shown in figure 4 after removal by EMR.
Source: UHBW NHS Foundation Trust.
The first step of the procedure is to check that there is no
sign of cancer invading the muscle layers. If this is the case, it
is not possible to remove the abnormal cells / cancer with an
endoscope. Furthermore, if there is a cancer that is advanced
enough that it invades a deeper layer; the risk of it spreading to
lymph glands nearby is over 50%. This would mean that in 1 of 2
patients, the treatment would not be curative. To check if there is
cancer invading the muscle, we inject a blue solution under the
mucosa to "lift" it away from the muscle. This not only confirms
that there is no attachment between the mucosa and the muscle, but
makes it safer to remove the mucosa.
As with any endoscopy, there are some risks. These include
making a hole in the oesophagus (perforation), or making the
oesophagus bleed. Bleeding is often minor and can be stopped at the
time of your procedure. After the procedure, there is a small risk
of scarring developing at the EMR site causing a narrowing that
makes it difficult to eat and drink normally. This may occur some
weeks after the procedure, but is rare. More information about
these and other risks are discussed in the EMR-specific booklet you
will be given on the day of your procedure, and will be discussed
with you on the day of your clinic appointment.
If you have had an EMR of a nodule in your Barrett's oesophagus,
the next step is to treat the rest of the Barrett's. This is done
using a technique called radiofrequency ablation or HALO. This is
scheduled for 8 weeks after your EMR to allow the gullet to heal.
For patients having EMR that completely removes the Barrett's, a
standard endoscopy under sedation or with throat spray is done to
check the EMR site has healed, again 8 weeks later.
Radio Frequency Ablation (RFA)
Radio frequency ablation is a treatment, which uses radio
frequency energy, a type of radiation similar to that used in
mobile phones, to produce a heating effect on the Barrett's cells
to destroy them (see figure 4). The treatment is delivered during
an endoscopy procedure under general anaesthetic and patients can
go home the same day. A thin probe is passed through the
endoscope which has a balloon at the end, wrapped in wires. Energy
is sent to the wires which heats them up. This burns only the
Barrett's cells in the affected part of the oesophagus. We use a
device that provides a burn through 360 degrees to the
circumference of the oesophagus.

Figure 4. Radiofrequency ablation device and diagram
illustrating its use in the lower oesophagus.
In some cases when the Barrett's is affecting a long stretch of
the gullet, we may decide to treat the Barrett's in 2 procedures to
minimise the risks.
As with EMR, this is a safe procedure but there are some risks
that you need to understand. These risks include making a hole in
the oesophagus (perforation) and bleeding. After the procedure,
there is a risk of scarring developing as the oesophagus heals,
causing a narrowing that makes it difficult to eat and drink
normally. This may occur some weeks after the procedure. More
information about the risks of the procedure will be discussed with
you in clinic and on the day of your procedure.
After we have treated the Barrett's, we will schedule a standard
endoscopy under sedation or throat spray 8 weeks after the RFA to
check there is no remaining Barrett's. If there is, it can be
treated with a device called Argon Plasma Coagulation (APC), which
is described below.
Argon Plasma Coagulation (APC)
Argon Plasma Coagulationis a treatment that uses a jet of argon
gas, together with an electric current to burn away small patches
of Barrett's cells in the oesophagus. The treatment is carried out
during an endoscopy and you will be given a sedative to make you
slightly sleepy during the procedure. The procedure takes about 20
minutes and patients can go home the same day.
Argon Plasma Coagulation is repeated every 8 weeks until any
remaining areas of Barrett's are destroyed. Some patients do not
need APC treatment or just one session, while others may need 2 or
more sessions. Once you have had an endoscopy showing complete
destruction of your Barrett's, we can move on to surveillance
endoscopy.
Surveillance
After treatment for Barrett's oesophagus with dysplasia you will
be advised to have an upper GI endoscopy and biopsies at regular
intervals to monitor the treated area. This is called surveillance.
Surveillance begins once we have confirmed that all the Barrett's
has been destroyed. The first two endoscopies are done at 6 monthly
intervals after the Barrett's is confirmed to have been destroyed
for 1 year. Then you will have annual endoscopies until 5 years
after completing treatment.
These endoscopies are done at the A414 Queens Day Unit in
Bristol by our team. This is because we have the necessary
expertise in treating this condition, we have access to your
previous treatment records, and we know which area to biopsy at
each endoscopy. If Barrett's returns, we have pathways and
procedures in place to effectively deal with that. We appreciate
that for some patients this may involve a lot of travelling. Please
feel free to raise this issue with a member of our team, including
your local Clinical Nurse Specialist, if you are finding it
difficult to make the journey. It may be possible to do some
endoscopies in South Bristol, Bath or Weston by members of our
surgical team if these would be more convenient.
After 5 years, you will be discharged back to the care of your
GP. You will not need any further Barrett's surveillance
endoscopies.
Anti-acid medication
People with dysplastic Barrett's oesophagus are advised to take
regular anti-acid medication, even if you do not have symptoms of
acid reflux.
The most commonly used drugs to lower acid levels are called
Proton Pump Inhibitors (PPIs). These include omeprazole and
lansoprazole, amongst others. These types of drugs are some of the
most widely used in the NHS because symptoms of acid reflux are so
common.
Lifestyle changes
Being overweight or obese is associated with reflux, Barrett's
oesophagus and oesophageal cancer. It is therefore important to
lose weight if you are overweight or obese.
Smoking cigarettes and drinking alcohol are also associated with
acid reflux. Stopping smoking and avoiding alcohol will help
control any symptoms and reduce the level of acid going back up
into the oesophagus.
Adopting these changes will also have an important beneficial
effect on your overall health.